The medical transcript is used to create proper billing and coding, as well as creating a medical history for the patient. The transcript should be free from errors; any error can create a claim rejection by the insurer. For instance, outsourcing is your best choice if you don’t have access to skilled billers and coders. It also reduces administrative burdens and encourages employees to deliver quality care.
Software ensures all the form fields are filled out and corresponding codes and fees make sense. Medical billing is a challenging and necessary component of today’s healthcare system. Handling and managing this process is a complicated task requiring experience to navigate each step successfully. But you should not be concerned about it because MedsIT Nexus Medical billing and coding services are 24/7 available for you with all the latest technologies and software.
How Not Paying Your Outstanding Provider/Hospital Bills Can Affect You?
If there are procedures or services that will not be covered, the patient is made aware that they will be financially responsible for those costs. One of the things that you may be curious about is how medical billing works, and how a claim moves through the medical system, the healthcare facility, and the insurance system. If a claim’s missing critical data or if it’s miscoded, it’ll be rejected and sent back to you. You can file an appeal, asking the insurance provider to reconsider its decision. If a third-party reviewer decides to favor the client, the health insurance company will pay for the treatments or services rendered.

It’s important for you as the provider to be aware of this step and to follow up as necessary to ensure you receive payment promptly. Each step in the process is crucial to the overall success of the medical billing process. The second step in the process is to determine financial responsibility for the visit. This means looking over the patient’s insurance details to find out which procedures and services to be rendered during the visit are covered.
What is Revenue Cycle Management?
They might reimburse you just a portion of the total amount you billed. They’re like that cool friend who always brings half the money for pizza. Simplifying the payment process for your patients helps encourage payments in full and on time. Self-service is key here—implementing a patient portal with an online payment system, for instance, allows your patients to pay their bills when and where it’s convenient for them to do so. The more barriers to payment you can remove, the less likely it will be for a patient statement to pass on to a collections agency.
- Your statement balance is calculated after each billing cycle by adding the transactions to your previous amount if there was one.
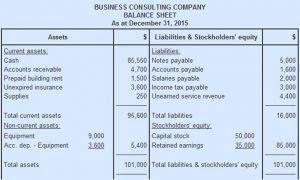
- Take a look at the table below to understand the distinctions between the two.
- Aside from actually rendering care, it is the most important part of keeping your practice alive and well.
- The financial health of physician practices and provider organizations, such as hospitals, health systems, and surgery centers depends on the effectiveness of front-end and back-end billing staff.
- Medical billing is a challenging and necessary component of today’s healthcare system.
- With healthcare continuing to have a high demand for qualified workers, many people are choosing medical billing and coding as a career.
- The superbill contains all of the necessary information about medical service provided.
Patient registration is the initial step in the revenue cycle management process. It involves collecting accurate and complete patient information, including demographic details, insurance coverage, and contact information. The challenges faced during patient registration include errors or omissions in data collection, which can lead to billing and reimbursement issues later in the process.
Step 5: Claims Submission
Once the insurance company chooses to pay the claims, they issue the money through a check or an electronic fund transfer. They also share a description known as an Explanation of Benefits (EOB) or an Electronic Remittance Advice (ERA). It is the responsibility of the professionals controlling the payment to publish the entries in the EHR and medical billing process count the payments received. This procedure is intricate and is governed by laws unique to payers and the states where providers are based. In reality, a claims appeal is the procedure a provider uses to get paid fairly for their services. Billers must make correct, “clean” claims because this procedure can be time-consuming and difficult.
A Trans Teen in an Anti-Trans State – The New Yorker
A Trans Teen in an Anti-Trans State.
Posted: Mon, 09 Oct 2023 07:00:00 GMT [source]
Once these final payments are made by patients, commonly arriving by mail, they should be posted and balanced. With many patient cases, this completes the billing process and closes the patient account. Clearinghouses, when used, typically offer dashboards that give billers convenient access to status updates for submitted claims.
